
Need help? You’re not alone. For free, confidential support available 24/7, call the 988 Suicide & Crisis Lifeline at 9-8-8 or visit 988lifeline.org. Whether you or someone you love is going through a tough time, help is just a call away. If you’re facing an emergency, please dial 911 or head to the nearest emergency room right away. Your well-being matters.
We recently released new data on our platform here at the Health Equity Tracker, shedding light on the tragic intersections of gun violence with homicides and suicides. September is National Suicide Prevention Month, a time when the nation reflects on the importance of prevention and mental health support. As someone who champions health equity through my work, this issue carries immense weight.
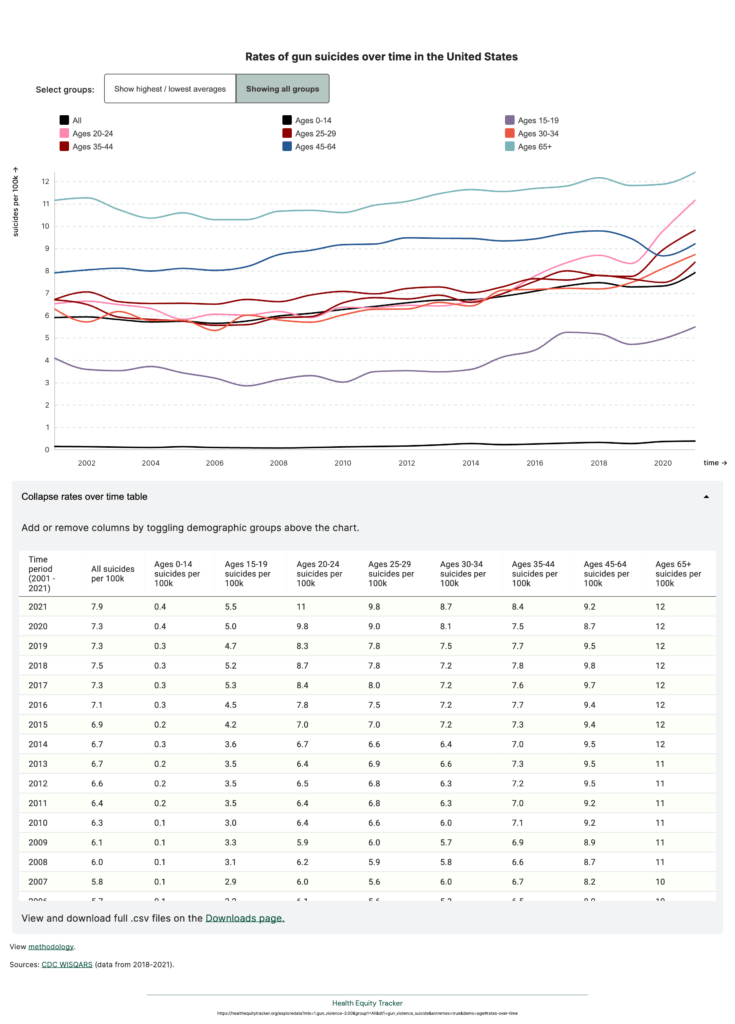
For me, and countless others who have experienced the devastating loss of a loved one to gun violence, this topic is deeply personal. Two years ago, my brother—an Airman, a father, and a husband—died by suicide using a gun. His death is part of a larger and disturbing trend. In the past decade, the suicide rate for 25- to 29-year-olds has risen from 6.8 to 9.8 per 100,000.
Like so many others in his age group, my brother was facing significant life transitions—pressure at work, financial stress as a new parent, and the weight of mental health struggles that were rarely discussed in our English as a Second Language (ESL) household. He had voluntarily sought inpatient treatment and had the support of therapy, medication, and social workers, but there were still gaps in the system. As a first-generation American from immigrant parents, the cultural disconnect of serving in the military on the mainland after growing up on an island his whole life added another layer of complexity to his struggles. Despite the efforts of his wraparound service team, the systems in place were simply not equipped to fully understand or address the unique intersection of his cultural, mental, and emotional needs. His story is a stark reminder that the rising suicide rates are not just a reflection of personal crises but of broader systemic failures—failures to provide truly comprehensive, culturally competent care, particularly for men and communities of color.
When we discuss gun violence and suicide, it’s critical not to reduce victims to mere statistics and generalizations. My brother, for instance, was a responsible gun owner. He was a trained marksman, a licensed firearm safety instructor, and had his weapons temporarily confiscated during his inpatient stay. But when he left the hospital, a hidden gun, one he had kept secret, allowed him to take his life. The intersection of mental health and access to firearms is a crucial one. Research shows that mental illness accounts for a significant portion of suicides, and firearm restrictions—such as those for people with a history of mental health challenges—can reduce suicide rates, particularly among men aged 25 to 44.
There is a broader systemic context to this issue. Gun violence and suicide are not just individual tragedies; they are deeply connected to structural inequities. Communities of color, in particular, often face disinvestment and lack of access to mental health resources. According to the FrameWorks Institute, one of the key drivers of gun violence is the lack of access to social supports. Without reliable safety nets, crises escalate into tragedies. This is why we must focus on solutions that improve access to social supports, particularly in systemically marginalized communities. Programs like hospital-based violence intervention can play a key role in reducing both gun violence and suicides by providing trauma-informed care to those who need it most.
At the Health Equity Tracker, our goal is to provide unbiased data to inform and enable the development of fair and effective policies. Understanding the data through a health equity lens means recognizing how systemic factors like inequitable resource allocation and the lack of legislative support for community-based interventions play a role in perpetuating these tragedies. It’s not enough to only discuss the mental health aspect of gun violence; we must also address the structural and policy failures that allow these preventable deaths to continue.
I write this not to sensationalize my brother’s death, but to illustrate that the data we provide on the Health Equity Tracker are not just numbers. They reflect real lives—lives that could be saved with the right policies, support systems, and community interventions. By elevating the voices of those directly affected by gun violence, we can work toward meaningful change that addresses the root causes of this public health crisis.
Explore our Policy Hub to discover how you can leverage the data on our platform to drive meaningful change and empower your community to take action.
From physicians to policymakers, our graduates lead across sectors—creating inclusive, evidence-based solutions that improve health outcomes in underserved communities. Become a changemaker today.
Contact Us