
I had the privilege of attending this year’s American Public Health Association conference in Washington, DC, with my esteemed colleagues from the Satcher Health Leadership Institute (SHLI). Shoutout to the Morehouse School of Medicine and the Annie E. Casey Foundation for helping us get there! There aren’t a ton of opportunities to travel as a tech person in the public health space, so I’m extra appreciative of everyone that made this conference trip happen. My fellow engineer at the Health Equity Tracker, Eric, had co-authored a poster alongside SHLI’s incredible Evan Martin, LCSW, that was accepted for presentation on Day 1 of the conference, titled, Understanding Geospatial Disparities in HIV Care and Prevention: Insights from the Health Equity Tracker.
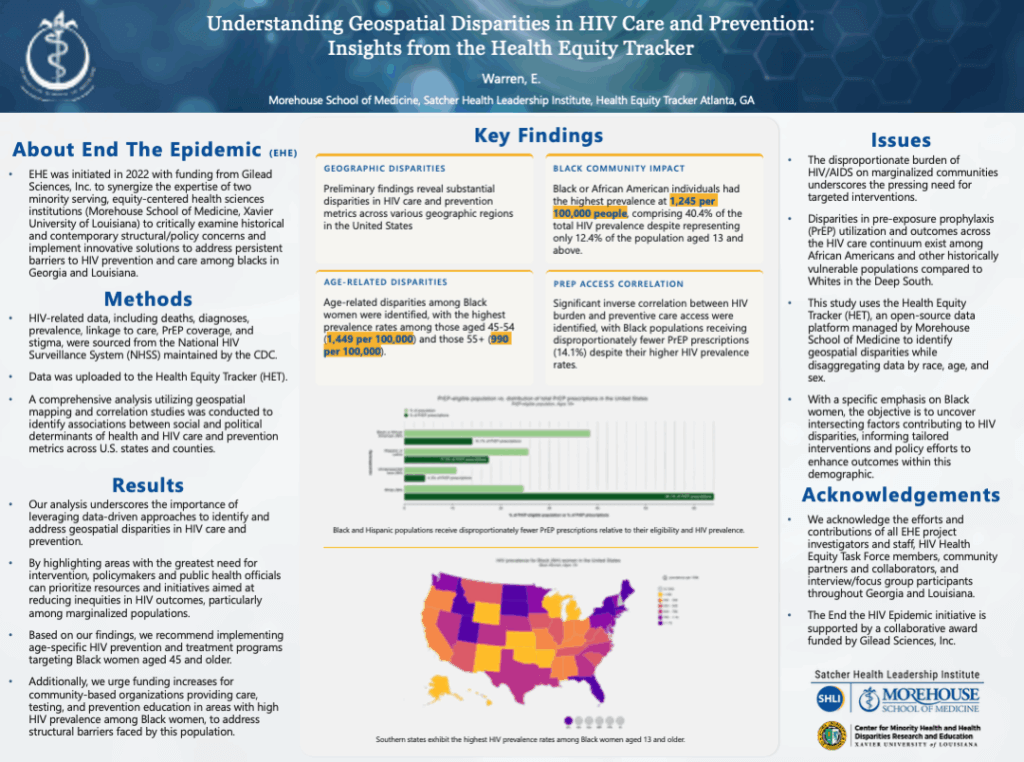
It was exciting being able to assist Eric with oncoming traffic and answering questions about the Tracker. I work with an amazing team on this app, and seeing other people “geek out” about the Tracker with me was an energizing experience. Here’s a bit more about the poster:
The poster revealed some stark realities about HIV in America. The data shows Black Americans face a massive HIV burden – they make up about 40% of all HIV cases despite being only 12% of the population. The real kicker? Black women aged 45-54 have particularly high rates of HIV, yet Black communities receive only 14% of PrEP prescriptions (that’s the preventive medication that can stop HIV transmission). This mismatch between who needs help and who’s getting it shows we need better prevention programs specifically designed for Black women over 45, plus more funding for community organizations in these high-need areas.
The presentation sessions were only for an hour, but the interactions with such esteemed public health professionals was ongoing.
Eric and I weren’t the only ones representing the SHLI at APHA! We had the wonderful Allyson Belton, MPH and Dr. Maisha Standier present their posters, Ending the HIV epidemic through health equity leadership development training and Up In Smoke and Age: Examining Medical Cannabis Perceptions on Use and Treatment of Chronic Pain in Older African American Patients in Georgia, respectively.

Eric was even able to connect IRL with one of our major sources of data, the America’s Health Rankings. He had the privilege of being one of their beta testers back in 2023 for their proprietary API they developed and now can showcase for all to use.
I got to meet some of the founding team members, Daniel E. Dawes, J.D. and Nelson J. Dunlap, responsible for the conception of the Tracker too. So many brilliant minds worked with Google.org back in 2020 to create this app that was once only a COVID-19 tracker, but now has over 60 different topics (and counting!) to choose from.
We attended a plethora of talks at this conference too. What stood out the most, though was seeing how our unique space that spans across public health, digital health, health equity, and in the works—AI— was being represented at this conference. I personally enjoyed one of the Health Informatics Information Technology (HIIT) roundtables on Public Trust, Health Informatics Competencies, Precision Prevention and more using Artificial Intelligence.
One table talked about Advancing trustworthy AI in under-resourced health systems: A community-informed approach. This table’s discussion was led by George Washington University School of Medicine & Health Sciences’ Senait Tekle, PhD. Dr. Tekle talked about a study on the the potential to improved healthcare delivery, with the use of AI. There was general interest in clinical care support, however, the trust in this delivery was mixed. I liked one quote from an Ethics Expert who participated in the study, who said, “Given that the medical literature is inherently biased, teaching AI off of existing literature will embed the same bias that’s currently present in the literature in AI.”
What really hit different about this quote is how it mirrors my own concerns about AI in healthcare. The humans teaching these models aren’t just coding – we’re literally shaping how future healthcare AI will “see” different communities. And here’s where it gets real: terms like “health equity” are becoming politically charged, and the DEI initiatives we’ve been building for the past decade are now under attack.
As developers who speak AI’s language, we’re at a crossroads. We can either let these models learn from the same biased playbooks that got us here, or we can be intentional about baking equity into the code from day one. The tech isn’t neutral – it’s only as inclusive as we make it. And honestly? With the current political climate trying to roll back progress on equity, our role as tech folks in public health has never been more crucial. We’re not just building apps; we’re building the future of healthcare access
The Health Equity Tracker isn’t just displaying data – it’s making inequities impossible to ignore. And that’s the energy we need to bring to every AI project touching healthcare. Because if we don’t advocate for equitable AI now, we’re basically cmd+c, cmd+v-ing discrimination into the future.

From physicians to policymakers, our graduates lead across sectors—creating inclusive, evidence-based solutions that improve health outcomes in underserved communities. Become a changemaker today.
Contact Us