If COVID-19 taught America anything, it is that good and current data is a significant piece of the health equity puzzle. We have seen that the lack of quality data around health equity and the analysis of the data are key to making the invisible visible.
Without data and tracking it is hard to know if the solutions that are being developed and implemented are having an impact. It took this global pandemic and the lack of solid data to show that we must be committed to digging deeper to uproot inequities if we are going to build a healthier America. There is no doubt that if we who work in the fields of academia, medicine, health policy, public health, nonprofits and community health activism are going to truly address and improve health inequities in this country, we must be able to aggregate, analyze and share health data at the local, state and national levels.
Just as the Health Equity Task Force helmed by the Satcher Health Leadership Institute, and their Health Equity Tracker is seeking to capture key and consistent data that will give us a better picture of disparities, the Commonwealth Fund partnered with the African American Research Collaborative (AARC), on the American COVID-19 Vaccine Poll to gain insight into what drives health care decisions and actions among people of color. This nationwide poll of more than 12,000 Americans inquired about COVID-19 vaccine uptake and access. The poll had the largest sample of African Americans, Latinos, Asian Americans, Pacific Islanders, and Native Americans of any study of COVID-19 vaccine uptake to date.
Our poll’s questions sought to find out how Americans, especially rural residents, people of color, and the unvaccinated, are currently thinking about the COVID-19 vaccines, what their concerns are, and what they think of having their children vaccinated and how those concerns might be addressed. While this information is important now, as it relates to getting as many people vaccinated as possible, to stem the tide on this pandemic, it also casts light on how we might approach health inequities more broadly and improved outcomes moving forward.
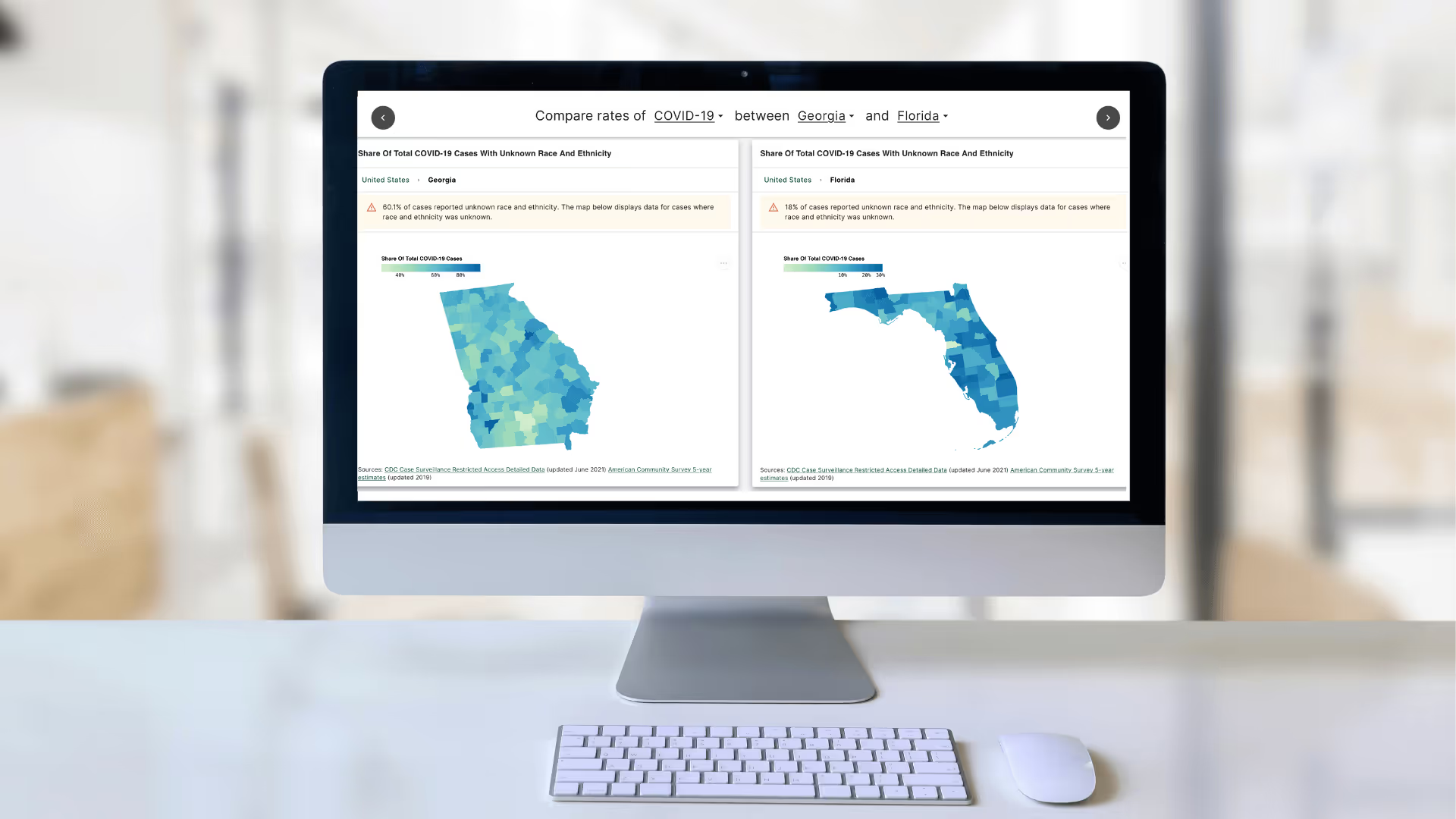
The pandemic also continues to show that there is a weak link of data collection, when it comes to the numbers of people who were diagnosed with COVID-19, the severity of their diagnosis, and the mortality rates. The Health Equity Tracker gives those who work in the field valuable data that can be used to shape policy, funding and targeted resources to bring about change. Our survey – by intentionally incorporating the voices and perspectives of people of color- adds another layer of depth to the conversations around vaccine equity—perceptions and how they translate into individual and community action (or lack thereof).
Our poll emphasizes that experiences of discrimination impact the way populations interact with systems of care. As an example, the poll’s questions sought to find out how Americans, especially rural residents, people of color, and the unvaccinated, are currently thinking about the COVID-19 vaccines, what their concerns are, and how they might be addressed. While this information is important now, as it relates to getting as many people vaccinated as possible and ending the pandemic, it also casts light on how we will approach health inequities and improved outcomes moving forward. The health disparities contributing to this burden are long-standing. Months since the first vaccinations became available, we still see the importance of providing credible information by credible providers to build vaccine confidence and counteract misinformation especially considering the impact of the Delta variant.
The pandemic continues to show that the weak links in data collection, when it comes to the numbers of people who are diagnosed with COVID-19, the severity of their diagnosis, and mortality rates. Our poll adds a layer of depth to the conversation—addressing the impact of health system experiences and testing messages that can affect perception across unvaccinated groups of people, and how these findings can translate into individual and community action (or lack thereof).
More than 40% of people of color who self-identified as vaccine hesitant indicated that they or a member of their household experienced discrimination in their interactions with the medical profession because of their race, ethnicity, or language. This poll emphasizes that these experiences impact the way people interact with systems of care.
Participants cited the experience of discrimination within the health care system as one reason why they have chosen not to get a COVID-19 vaccine and how they make other health decisions. 27% of Black and 22% of Native American respondents indicated that they believe discrimination from medical professionals against their racial/ethnic group makes it hard to trust that COVID-19 vaccines are safe and effective for themselves and others from their community. The health disparities contributing to this burden are long-standing. More survey participants cited the current day experience of discrimination as a more significant factor in their vaccine hesitancy that the historical knowledge of the Tuskegee syphilis experiments. This points to the urgent need to take action to counteract inequities in health outcomes and treatment. Further partnership and community building between the medical and public health community and patients of color are needed.
While survey results give us insights into where we are in managing this pandemic, they also tell us some important things about how we all move forward with providing affordable access to care, addressing health status and ways to improve interaction with providers among underserved, minoritized and marginalized populations in the future. Our survey shows that more than half (53%) of all unvaccinated people would prefer to get vaccinated at their personal doctor’s office, with modest variation by race, ethnicity, and residence. Additionally, not having health insurance is major obstacle to the vaccine- with only 24% of the uninsured reported being vaccinated.
These findings call for ways to address risk factors for, and better management of, chronic conditions moving forward. We can start by strengthening access to care and primary care systems.
We do know from previous Commonwealth Fund surveys that adults in the U.S. experience greater affordability barriers to accessing physician visits, tests, and treatments. Increasing access to affordable health care and strengthening primary care systems are two of the most important challenges for the U.S. health care system.
This is a time for all of us to work together to ask the key questions, gather standardized data on key health issues, and get insights on how we can turn the tide on decades of discrimination and inequity and distrust that keep minoritized and marginalized people out of care and distanced from optimal health and wellness as we navigate COVID-19 and beyond.
From physicians to policymakers, our graduates lead across sectors—creating inclusive, evidence-based solutions that improve health outcomes in underserved communities. Become a changemaker today.
Contact Us